Amerigroup Pharmacy Prior Authorization Form 2019-2024 free printable template
Show details
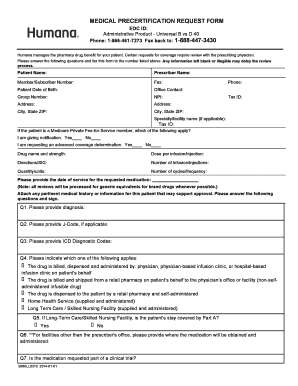
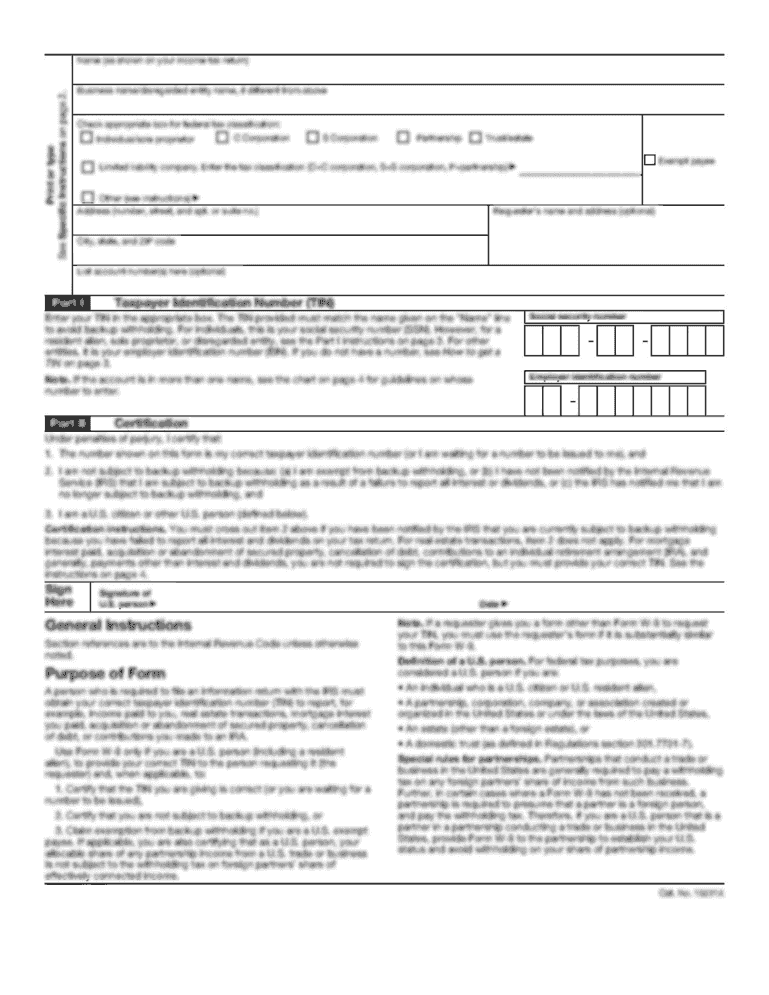
Pharmacy Prior Authorization Form INSTRUCTIONS Complete this form in its entirety. Any incomplete sections will result in a delay in processing. We review requests for prior authorization based on medical necessity only. We will notify the provider and the member s pharmacy of our decision. To help us expedite your authorization requests please fax all the information required on this form to 1 800 359 5781. Allow us at least 24 hours to review this request. If you have questions regarding...
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign
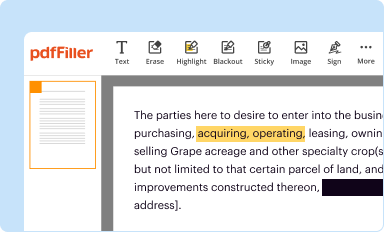
Edit your pharmacy prior authorization form form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
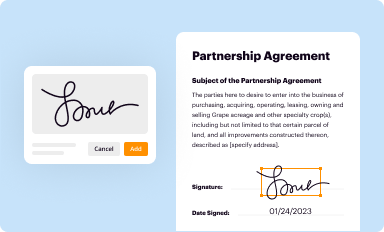
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
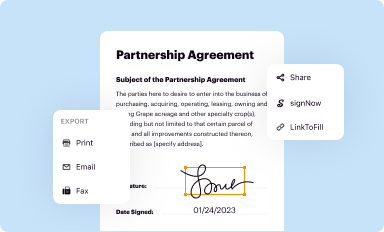
Share your form instantly
Email, fax, or share your pharmacy prior authorization form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
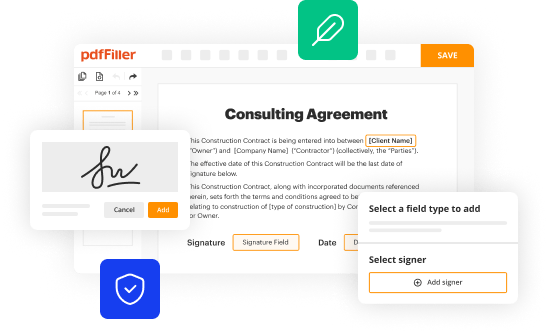
How to edit pharmacy prior authorization form online
Follow the guidelines below to take advantage of the professional PDF editor:
1
Log into your account. It's time to start your free trial.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit amerigroup prior auth form. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
With pdfFiller, it's always easy to work with documents.
Amerigroup Pharmacy Prior Authorization Form Form Versions
Version
Form Popularity
Fillable & printabley
How to fill out pharmacy prior authorization form
How to fill out a pharmacy prior authorization form?
01
Obtain the form: Start by obtaining the pharmacy prior authorization form from your insurance provider or healthcare professional. They can usually provide this form either in person or online.
02
Personal Information: Fill in your personal information accurately, including your full name, date of birth, address, and contact details. Make sure to double-check the information for any errors.
03
Prescribing Physician Information: Provide the necessary details of your prescribing physician, such as their name, address, and contact information. This information is crucial to ensure effective communication between the pharmacy and your doctor.
04
Patient Information: If the prior authorization form is for someone other than yourself, provide the patient's information, including their full name, date of birth, and contact details.
05
Prescription Details: Enter the necessary information about the medication requiring prior authorization. This includes the medication name, dosage, strength, and the reason why you need this specific medication prescribed by your doctor.
06
Supporting Documentation: Check if any supporting documentation is required, such as medical records, test results, or letters of medical necessity. Make sure to include these documents with your completed form to strengthen your case for the medication's necessity.
07
Healthcare Professional's Signature: If the form requires a healthcare professional's signature, ensure that your prescribing physician or healthcare provider signs and dates the form appropriately. This signature verifies that they are requesting the medication and supports your prior authorization request.
08
Submitting the Form: After completing the form and gathering any necessary supporting documentation, follow the instructions provided on the form regarding submission. Submit the form as instructed, whether it is through mail, fax, or electronically.
Who needs pharmacy prior authorization form?
01
Patients seeking medications: Individuals who require certain medications that are not commonly covered by their insurance plans may need to complete a pharmacy prior authorization form. This form allows their insurance provider to evaluate the medical necessity of the prescribed medication before approving coverage.
02
Healthcare professionals: Prescribing physicians or healthcare providers must initiate the prior authorization process for their patients, especially when prescribing medications that require additional documentation or justification. They need to complete the prior authorization form to ensure their patients have access to the prescribed medication.
03
Insurance providers: Pharmacy prior authorization forms serve as a tool for insurance providers to assess the appropriateness and medical necessity of certain medications. By reviewing these forms, insurance providers can determine if the prescribed medication aligns with their coverage policies before approving or denying the request.
Fill amerigroup pa form : Try Risk Free
People Also Ask about pharmacy prior authorization form
Who handles submitting a request for prior authorization?
What is prior authorization in pharma?
Who is responsible for authorization?
Why does Adderall require prior authorization?
Who sends the prior authorization form?
How do I write a prior authorization request?
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is pharmacy prior authorization form?
A pharmacy prior authorization form is a document that must be completed by a physician or other healthcare provider to request approval from a health insurance provider for a patient to receive a prescribed medication. The form is used to confirm that the medication is medically necessary and is covered by the patient's plan. It also includes information about the patient's medical history and other relevant information to help the insurer make a decision.
What is the purpose of pharmacy prior authorization form?
The purpose of a pharmacy prior authorization form is to provide information to a health insurer that is necessary to determine whether a medication is medically necessary and should be covered under the patient's health plan. This form helps the insurer make an informed decision about whether to approve or deny coverage for the prescribed medication.
What information must be reported on pharmacy prior authorization form?
1. Patient name and contact information, including date of birth.
2. Prescriber name and contact information.
3. Name of prescribed medication.
4. Dosage and strength of prescribed medication.
5. Frequency and duration of use.
6. Reason for the prescription.
7. Details of any other drugs being taken by the patient.
8. Requested quantity of medication.
9. Any relevant medical history, allergies, or other conditions.
10. Insurance information, including policy number.
When is the deadline to file pharmacy prior authorization form in 2023?
The exact deadline for filing pharmacy prior authorization forms in 2023 will depend on the particular form and the pharmacy in question. Generally, prior authorization forms must be submitted at least 10 days, but no more than 30 days, prior to the requested start date for the medication.
What is the penalty for the late filing of pharmacy prior authorization form?
Penalties for late filing of a pharmacy prior authorization form vary depending on the particular situation, and could range from a warning to a fine or other disciplinary action.
Who is required to file pharmacy prior authorization form?
Pharmacy prior authorization forms are typically required to be filed by pharmacists or pharmacy technicians. They are responsible for submitting these forms to insurance companies or healthcare providers to obtain approval for certain medications or services.
How to fill out pharmacy prior authorization form?
Filling out a pharmacy prior authorization form may vary slightly depending on the specific form provided by your insurance company or the pharmacy. However, here is a general step-by-step guide to help you navigate the process:
1. Obtain the form: Contact your insurance company, pharmacy, or healthcare provider to obtain the specific prior authorization form.
2. Read the instructions: Carefully read through the form's instructions to understand the information and documentation required for submission.
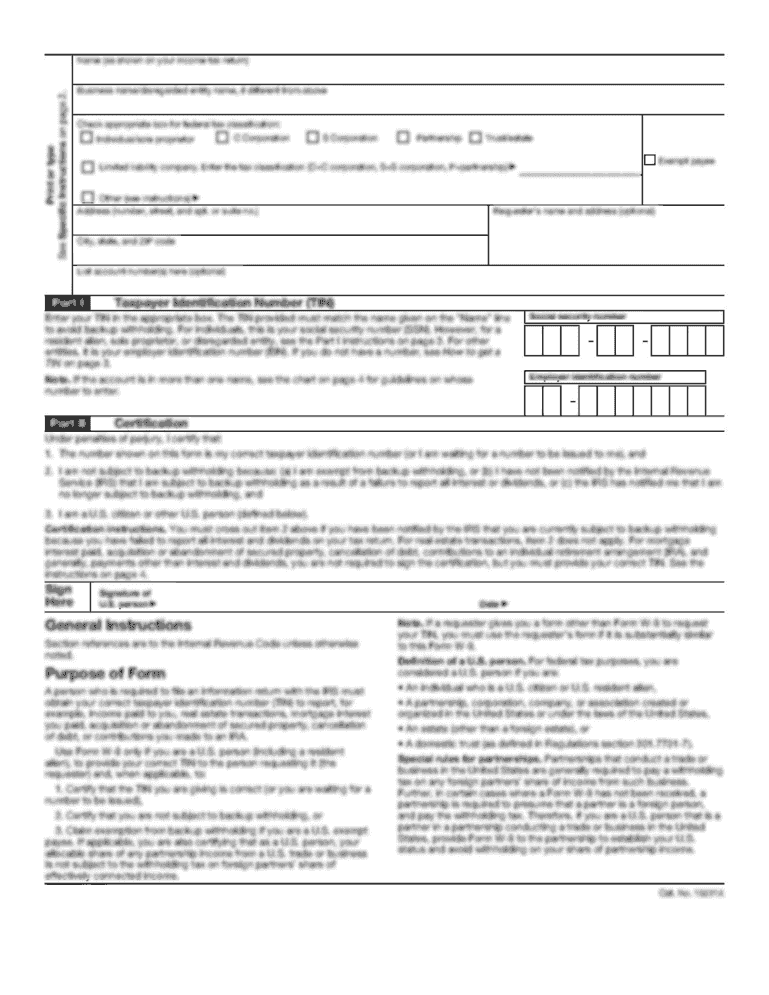
3. Complete patient information: Fill out the patient's personal information section, including their full name, date of birth, contact details, and insurance information. Ensure all information is accurate and up-to-date.
4. Include healthcare provider information: Provide the name, contact details, and credentials of the healthcare provider requesting the prior authorization. This may include the physician, nurse practitioner, or pharmacist.
5. Identify the medication: Clearly list the medication requiring prior authorization. Include the brand and generic name, strength, dosage form, and quantity.
6. Provide diagnosis and medical necessity: Document the patient's diagnosis, the reason the medication is necessary, and any relevant supporting medical information. This may include previous treatment modalities, failed alternatives, and any specific considerations.
7. Attach supporting documentation: Collect any supporting documentation required by your insurance company. This may include medical records, lab results, prescription history, or clinical guidelines. Ensure all pages are legible, labeled, and securely attached to the form.
8. Complete sections related to insurance coverage and benefits: Answer all questions related to insurance coverage, including out-of-pocket expenses, deductibles, and maximum coverage limits.
9. Review and sign the consent section: Read through the consent section carefully and sign to authorize the release of medical information for the purpose of prior authorization.
10. Submit the form: Make a copy of the completed form for your records, then submit the original form, along with any supporting documentation, to your healthcare provider, insurance company, or pharmacy. It is recommended to submit the form via certified mail or trackable delivery to ensure it reaches the intended recipient.
11. Follow up: After submitting the prior authorization request, follow up with your healthcare provider or insurance company to track the progress of the request. Keep a record of any communication, including dates, times, and persons contacted.
Remember that specific forms and requirements may vary depending on your insurance plan, so it's essential to carefully review the provided instructions and seek any additional guidance from your healthcare provider or insurance company if needed.
How do I make edits in pharmacy prior authorization form without leaving Chrome?
Install the pdfFiller Google Chrome Extension in your web browser to begin editing amerigroup prior auth form and other documents right from a Google search page. When you examine your documents in Chrome, you may make changes to them. With pdfFiller, you can create fillable documents and update existing PDFs from any internet-connected device.
How do I edit amerigroup authorization form straight from my smartphone?
The pdfFiller mobile applications for iOS and Android are the easiest way to edit documents on the go. You may get them from the Apple Store and Google Play. More info about the applications here. Install and log in to edit amerigroup prior authorization form.
How do I complete amerigroup pharmacy prior authorization form on an Android device?
Complete amerigroup authorization form and other documents on your Android device with the pdfFiller app. The software allows you to modify information, eSign, annotate, and share files. You may view your papers from anywhere with an internet connection.
Fill out your pharmacy prior authorization form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Amerigroup Authorization Form is not the form you're looking for?Search for another form here.
Keywords relevant to amerigroup prior authorization form pdf
Related to amerigroup pre auth form
If you believe that this page should be taken down, please follow our DMCA take down process
here
.